Personality Disorders
Personality Disorders Personality disorders are a group of a 10 mental health conditions that involve long-la sting, disruptive patterns of thinking, behaviour, mood and relating
Personality Disorders Personality disorders are a group of a 10 mental health conditions that involve long-la sting, disruptive patterns of thinking, behaviour, mood and relating
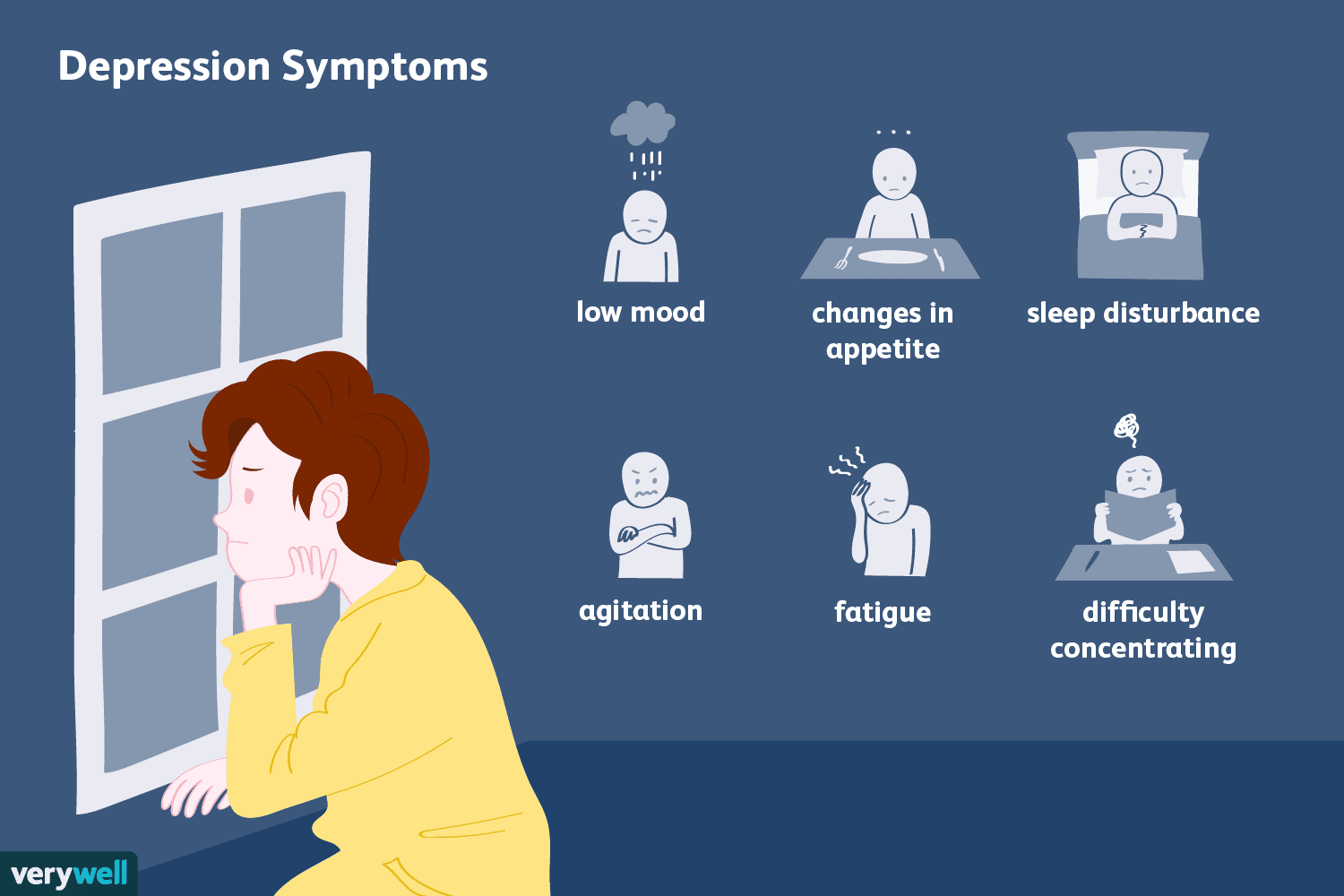
What is depression? Depression is one of the most common types of mental health conditions and often develops alongside anxiety. Depression can be mild and

COCAINE ADDICTION IN OVERSEAS PAKISTANI FAMILIES AND TREATMENT EXPERIENCE AT NEW HOPE REHAB CENTER ISLAMABAD What Is Cocaine Addiction? People who are struggling with cocaine

BEST REHABILATATION CENTER IN ISLAMABAD BENEFITS OF REHABILATATION FOR PEOPLE What is rehabilitation? Rehabilitation is care that can help you get back, keep, or improve
Copyright © 2024 rehab All rights reserved. Developed, SEO & Digital Marketing By: Web Technologies Pakistan
WhatsApp us