BORDERLINE PERSONALITY DISORDER
NEW HOPE REAHAB AND CARING CENTER ISLAMABAD
Borderline personality disorder is a mental illness that severely impacts a person’s ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others.
Signs and Symptoms:
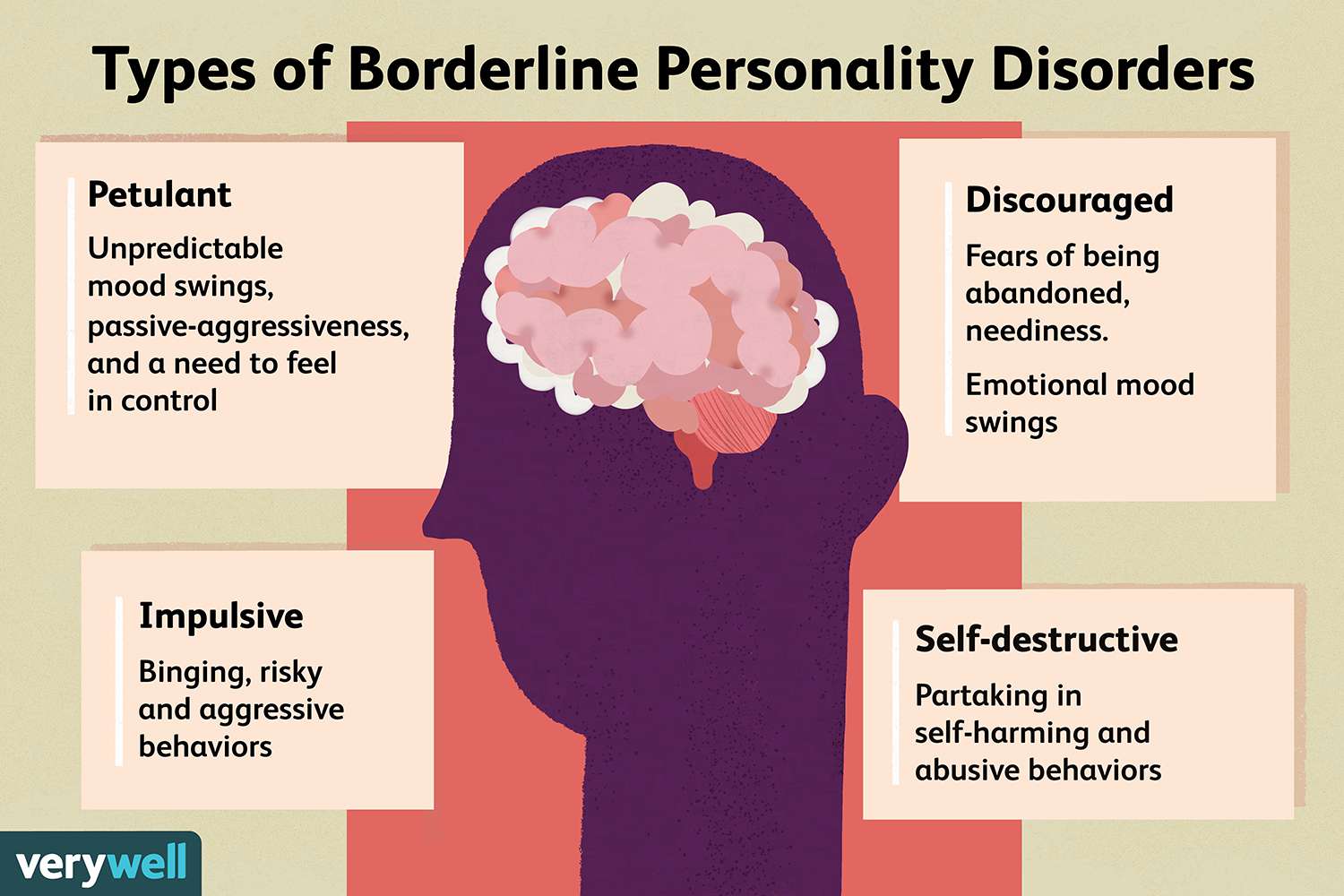
People who have borderline personality disorder may go through severe mood swings and struggle with their self-image. They have the ability to abruptly go from intense closeness to intense hate of others. Instable relationships and emotional suffering can result from these shifting emotions.
People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their interests and values can change quickly, and they may act impulsively or recklessly.
Other signs or symptoms may include:
- Efforts to avoid real or perceived abandonment, such as plunging headfirst into relationships—or ending them just as quickly.
- A pattern of intense and unstable relationships with family, friends, and loved ones.
- Impulsive and often dangerous behaviours, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviours happen mostly during times of elevated mood or energy, they may be symptoms of a mood disorder and not borderline personality disorder.
- Self-harming behaviour, such as cutting.
- Recurring thoughts of suicidal behaviours or threats.
- Intense and highly variable moods, with episodes lasting from a few hours to a few days.
- Inappropriate, intense anger or problems controlling anger.
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality.
- Chronic feelings of emptiness.
Risk Factors:
Family history:
People who have a close family member (such as a parent or sibling) with the illness may be at a higher risk of developing borderline personality disorder.
Brain structure and function:
Research shows that people with borderline personality disorder may have structural and functional changes in the brain, especially in the areas that control impulses and emotion regulation. However, the studies do not demonstrate whether these changes were risk factors for the illness or if such changes were caused by the disorder.
Environmental, cultural, and social factors:
Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or hardship during childhood. Others may have been exposed to unstable, invalidating relationships or conflicts.
Diagnosis:
Borderline personality disorder can be identified by a thorough interview and discussion of symptoms by a qualified mental health professional with experience in diagnosing and treating mental disorders, such as a psychiatrist, psychologist, or clinical social worker. A comprehensive medical examination can also aid in excluding other potential causes of symptoms. Providers will talk about a person’s symptoms and inquire about their family’s medical histories, including any history of mental illness.
Early adulthood or late youth are the typical diagnosis times for borderline personality disorder. Occasionally, if symptoms are severe and persist for at least a year, a person under the age of 18 may be identified as having borderline personality disorder.
What other illnesses can co-occur with borderline personality disorder?
Other mental diseases, such post-traumatic stress disorder, frequently co-occur with borderline personality disorder In particular, if symptoms of other illnesses match with those of borderline personality disorder, these co-occurring disorders might make it more difficult to identify and treat borderline personality disorder. The signs of serious depression, PTSD, bipolar disease, anxiety disorders, substance misuse, and eating disorders, for instance, may all be more prevalent in someone with borderline personality disorder.
Treatments and Therapies:
Borderline personality disorder historically has been viewed as challenging to treat. But with newer, evidence-based treatment, many people with this disorder experience fewer and less severe symptoms, improved functioning, and better quality of life. It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
Many factors affect the length of time it takes for symptoms to improve once treatment begins. It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
Psychotherapy:
Psychotherapy, sometimes called “talk therapy,” is the first-line treatment for people with borderline personality disorder. Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Dialectical Behaviour Therapy (DBT):
This treatment was developed specifically for individuals with borderline personality disorder. DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviours, and improve relationships.
Cognitive Behavioral Therapy (CBT):
This treatment can help people identify and change core beliefs and behaviours that come from inaccurate perceptions of themselves and others and problems interacting with others. It may help people reduce mood swings and anxiety symptoms and may reduce the number of self-harming or suicidal behaviours.
Medications:
Because the benefits of prescription medication for borderline personality disorder are unclear, medications aren’t typically used as the primary way to treat the illness. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms or co-occurring mental disorders such as mood swings or depression. Treatment with medications may require coordinated care from more than one medical professional.
Other Elements of Care:
Some people with borderline personality disorder experience severe symptoms and need intensive, often inpatient, care. Others may use some outpatient treatments but never need hospitalization or emergency care.
Therapy for Caregivers and Family Members:
Having a relative or loved one with the disorder can be stressful, and family members or caregivers may unintentionally act in ways that can worsen their loved one’s symptoms.
- Allowing the relative or loved one to develop skills to understand and support a person with borderline personality disorder.
- Focusing on the needs of family members to help them understand the obstacles and strategies for caring for someone with the disorder.
Common in which gender:
Borderline personality disorder is common in females than men’s.
TREATMENT AT NEW HOPE:
In new hope rehab centre healthcare provides will suggest a treatment plan based on the person’s symptoms. The new hope team carefully plan a treatment. A psychiatrist and physician plan a medication and a skilful psychologist provide psychotherapy.
Psychotherapy can be important treatment component for people with borderline personality disorder. It can enable them to recognize changes in thoughts and mood and respond accordingly.
Our New Hope team aim is to provide awareness regarding mental health general and specifically borderline personality and other mental health disorders.
About the author:
Laiba Shahab: Clinical Psychologist at New Hope Rehab and caring centre.
She can be reached at:
laibashahabuddin@gmail.com.
HOUSE # 275, STREET 2, BLOCK A, NEAR SAVE MART, SECTOR O9, NATIONAL POLICE FOUNDATION, ISLAMABAD
CONTACT NO, 0312-7493940, 0333-9040005, O51-882631