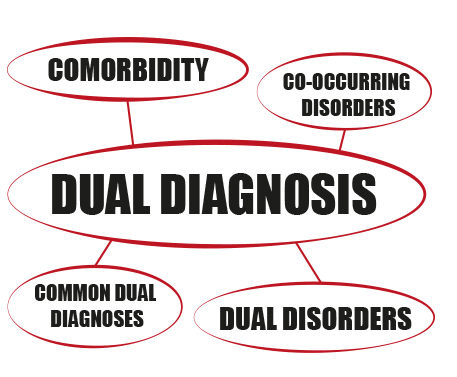
DUAL DIAGNOSIS AND ITS CHALLENGES
A person with dual diagnosis has both a mental disorder and an alcohol or drug problem. These conditions occur together frequently. About half of people who have a mental disorder will also have a substance use disorder at some point in their lives and vice versa.
Example of dual diagnosis:
Dual diagnosis is having a combination of drug addiction and mental illness. For example, you can struggle with depression and alcoholism concurrently. If not addressed, these disorders may worsen each other.
What is the most common dual diagnosis?
5 Most Common Co-Occurring Disorders
1 – Generalized Anxiety Disorder (GAD)
2 – Attention Deficit Hyperactivity Disorder
3 – Post Traumatic Stress Disorder
4 – Clinical Depression
5 – Bipolar Disorder
Co-occurring disorders or comorbidity are other terms that may be used to describe dual diagnosis. Comorbidity is the term used to indicate the presence of two or more disorders in the same person. They could take place simultaneously or one after the other. Comorbidity also denotes interactions between the diseases that could make both of them worsen.
Symptoms of Dual Diagnosis
- Distance from friends and family.
- A sudden change in behaviour.
- Abusing Using substances using even in unsafe conditions.
- Risk-taking behaviour.
- The need to use taking control.
- Higher tolerance and more significant withdrawal symptoms.
- Unable to function without the preferred drug.
What is the importance of dual diagnosis?
Dual diagnosis occurs in different forms when any mental illness (such as anxiety, depression, and psychosis) combines with an addiction (such as an alcohol use disorder). The importance of dual diagnosis treatment is evident for people who are struggling with multiple mental health illnesses.
How do you treat a dual diagnosis?
An integrated strategy, in which both the mental health issue and the substance use issue are treated concurrently and by the same treatment provider or team, is the best course of action for dual diagnosis.
What is dual diagnosis in DSM?
Definition.
Dual diagnosis is the term used to describe patients with both severe mental illness (mainly psychotic disorders) and problematic drug and/or alcohol use.
How do you deal with dual diagnosis?
When a person receives therapy for both their identified mental illness and substance dependence, integrated intervention is the optimal form of treatment for dual diagnoses. The notion that “I cannot treat your depression because you are also drinking” is outmoded; modern thinking calls for treating both problems simultaneously.
Reasons for Treating Co-Occurring Disorders Differently. 45 percent of Americans struggle with a dual diagnosis, according to the NSDUH. About two times as often people with mental health diagnoses have an SUD as the general population.
What is dual diagnosis in disability?
First utilised in the USA during the 1970s, dual diagnosis was used to describe mental health problems in adults with an intellectual disability. The term, dual diagnosis, specifically refers to co-existing intellectual disability and mental disorder.
Today, dual diagnosis treatment is the term most often used to describe how those who have both a mental illness and addiction are treated. Co-occurring disorders describe a variety of diseases that commonly occur along with drug abuse or alcohol addiction.
DUAL DIAGNOSIS EFFECT FAMILY
The impact of the dual diagnosis will often result in families being called upon financially to support the person. Rent, clothing, haircuts and transport all become less of a priority and families are put in the difficult position of making up this shortfall or having their family member suffer the consequences.
Dual diagnosis was first identified in the 1980s among individuals with coexisting severe mental illness and substance abuse disorders. Today, the Substance Abuse and Mental Health Services Administration (SAMSHA) uses the term co-occurring disorders (COD) to refer to the aforementioned concurrent disorders.
The consequences of dual diagnosis include poor medication compliance, physical comorbidities and poor health, poor self-care, increased suicide risk or aggression, increased sexual behaviour, and possible incarceration.
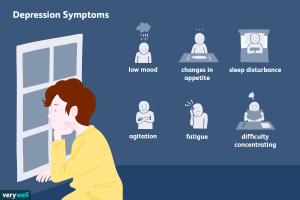
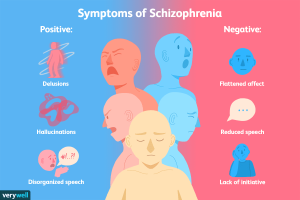
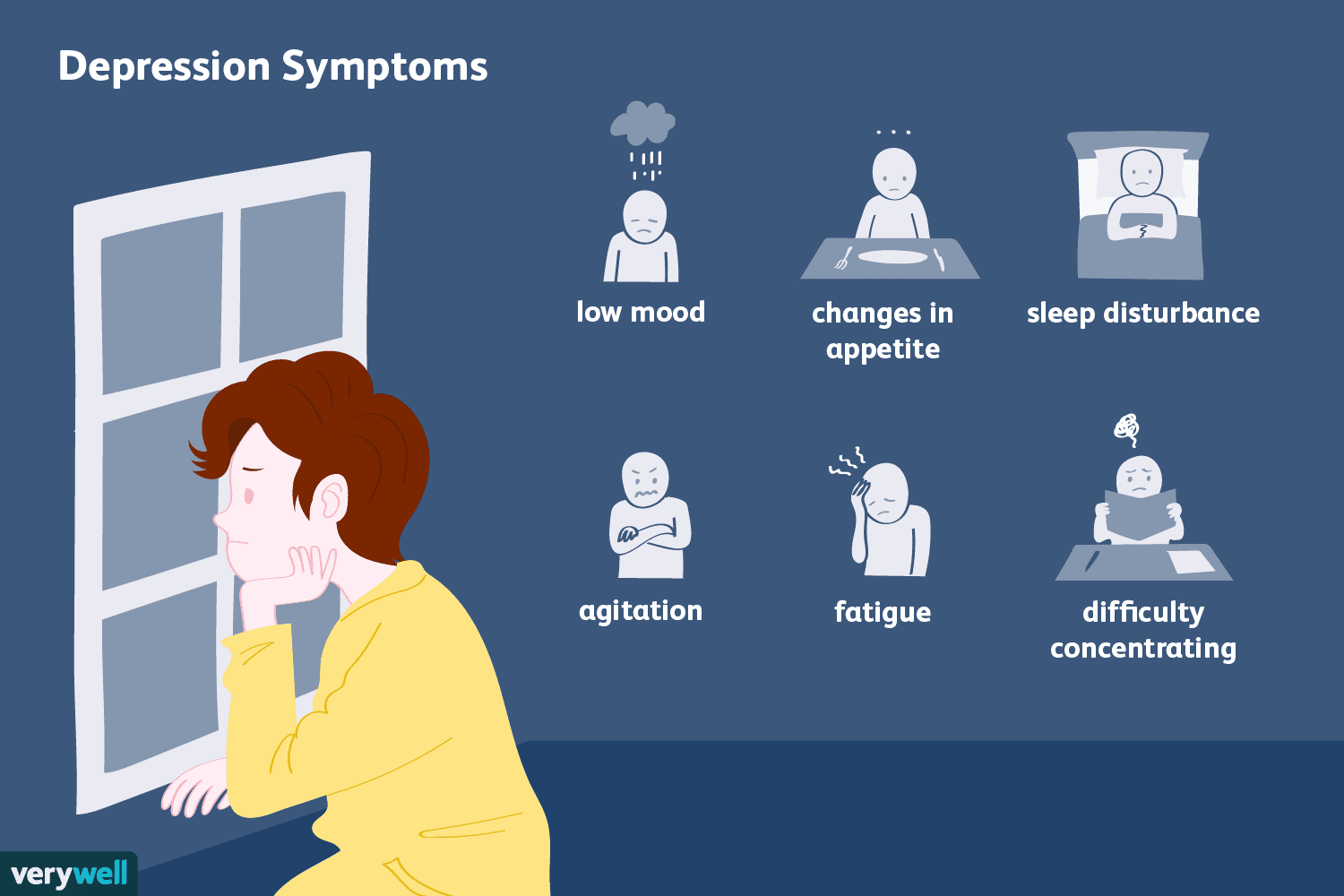
Symptoms of a mental health disorder may include:
- Extreme mood changes.
- Problems concentrating.
- Unable to function at work or school.
- Avoiding social activities.
- Thoughts of suicide.
- Confusion
Which disorder comes first in a dual diagnosis?
Like the chicken or the egg, it can be difficult to figure out which came first. Even though dual diagnoses occur together, it doesn’t mean one caused the other.
Substance use disorders may not directly cause mental health disorders (or vice versa), but there’s a clear connection between the two. Drugs and alcohol can worsen the symptoms of mental health conditions. And the continued use of these substances can increase your risk of developing a mental health disorder.
Shared common risk factors
Genetics:
Mental health disorders and substance use disorders can both run in families. Research shows many genes may contribute to your risk of developing either condition.
Environmental factors:
Environmental factors such as stress and trauma can be passed down through generations. These can contribute to the development of a substance use disorder or a mental health disorder.
How is dual diagnosis diagnosed?
Dual diagnosis isn’t a diagnosis — it’s a combination of diagnoses. It can be difficult for your healthcare provider to make an accurate diagnosis because the symptoms of both disorders can overlap.
However, your provider will use wide-ranging screening tools to evaluate you for both disorders. It’s important to be honest when speaking with your healthcare provider. Based on your answers, they can determine which disorders you may have and identify appropriate treatment.
What is dual diagnosis treatment?
Dual diagnosis treatment will include treatment for your mental health condition and your substance use disorder at the same time. You’ll work with your healthcare provider to understand the ways each of your disorders affects the other. This will help you determine which treatment will be most effective.
For you to achieve a dual diagnosis recovery, you must stop using the addictive substance. For many people, this may start with detoxification. During inpatient detoxification, healthcare providers will monitor you 24 hours a day for up to a week. They’ll help you wean off the substance and provide ways to lessen the effects of withdrawal.
Behavioral therapy
Behavioral therapies that have been shown to treat co-occurring disorders include:
Cognitive behavioral therapy (CBT):
Cognitive behavioral therapy can teach you how to cope with and change ineffective patterns of thinking.
Dialectical behavioral therapy (DBT):
Dialectical behavioral therapy can reduce self-harm behaviors. These may include drug use, cutting and suicidal thoughts or actions.
How can I reduce my risk of dual diagnosis?
- Learning about your biological family history.
- Limiting the amount of alcohol you consume.
- Talking to your healthcare provider.
TREATMENT IN NEW HOPE:
In new hope rehab centre healthcare provides will suggest a treatment plan based on the person’s symptoms. The new hope team carefully plan a treatment. A psychiatrist and physician plan a medication and a skilful psychologist provide psychotherapy
Our new hope team aim is to provide awareness regarding mental health general and specifically dual diagnosis and other mental health
ABOUT THE AUTHOR:
LAIBA SHAHAB: Clinical psychologist at NEW HOPE REHAB AND CARING CENTER
She can be reached at:
ADDRESS:
House 275, street 12, block A, Near save mart national police foundation 0-9 Islamabad
CONTACT NO, 0312-7493940, 0333-9040005, O51-882631